Dysphagia is the medical term for swallowing difficulties. It can be caused by a range of conditions, such as cancer, head injuries, a stroke or dementia. Depending on the severity of their dysphagia, a care home resident may find some textures hard to swallow or may have lost the ability to swallow at all, which makes eating difficult. Knowing what dysphagia is and how to best support someone with it is therefore vital – the condition must be carefully managed to prevent malnourishment and more extreme medical problems.
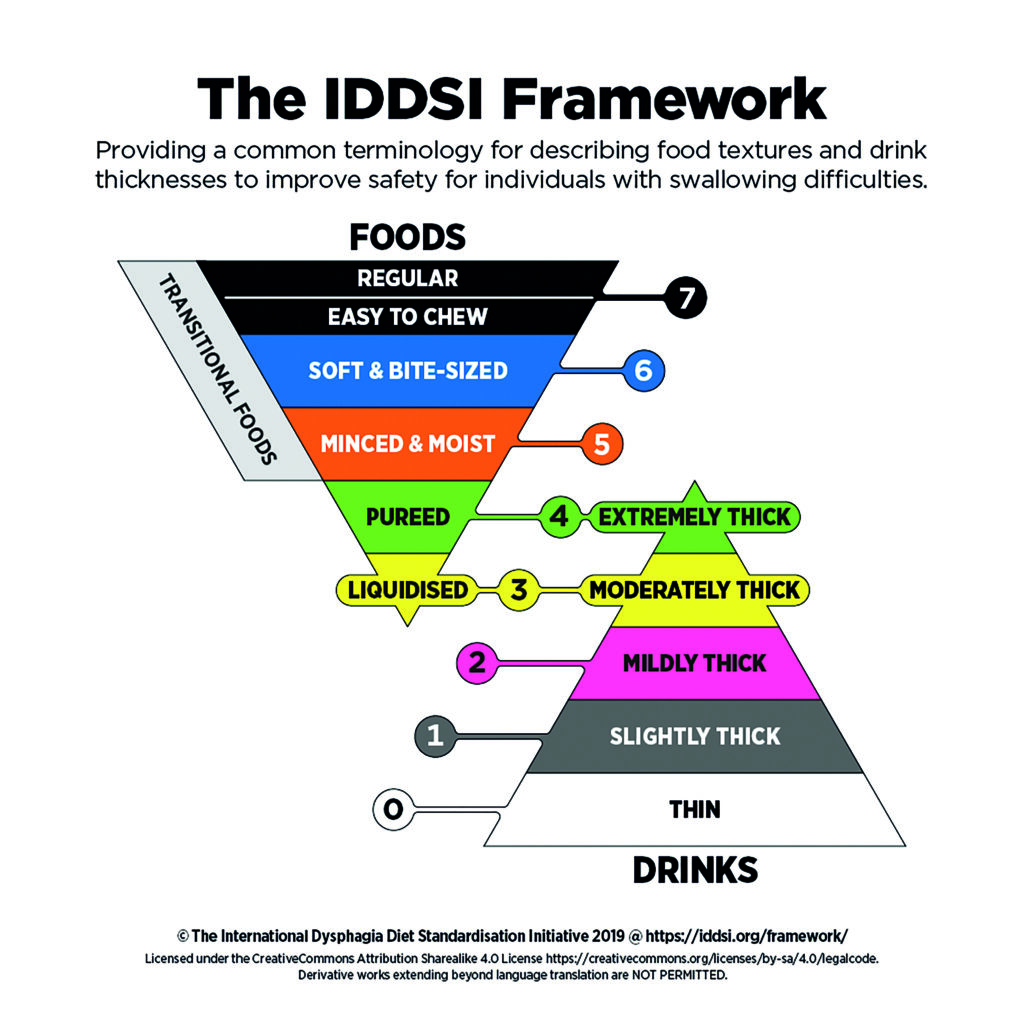
The IDDSI Framework
The International Dysphagia Diet Standardisation Initiative (IDDSI) gives mandatory guidelines for caterers on how to provide the right dietary support for residents with dysphagia. Under these guidelines, all food and fluids are graded on a 0-7 scale based on their viscosity, with zero being the lowest such as water, and seven referring to easy-to-chew foods.
Leni Wood, Head of Nutrition and Wellness at Nellstar, highlights how instrumental these guidelines are in their kitchens: “We have staff in some homes whose first language is not English, who find it easier to read and understand information in their first language. I can easily direct them to the IDDSI guidance in any language and they can read how to comply. I always say to everyone, the IDDSI framework is
your bible when it comes to knowing the texture modified levels and we can all follow what is written.”
Having the correct equipment to modify food is essential. For example, the chefs at Aria Care adapt their method for modifying texture depending on the IDDSI scale, using a Thermomix machine for levels 3, 4 and 5 and a fork for level 6 to crush food into soft and bite-sized 1.5cm x 1.5 cm cubes.
The IDDSI guidelines make it easy for chefs to texture-check prepared foods, however for testing liquids, two syringes must be used to test the flow rate. Once the tools are in place, it’s crucial that all catering staff are trained to the same level. “Thanks to continuous training, at Aria our chefs are able to reverse engineer our menus, so all residents have the opportunity to eat the same thing – preventing anyone from feeling isolated or different – and we encourage anyone supporting residents with dysphagia to do the same.
There are no limitations to what someone with dysphagia can eat – they need to eat a full, nutritious and balanced diet, just like everyone else and the IDDSI guidelines help us to deliver just that,” comments
James Clear, hospitality director, Aria Care.
When a resident has been assessed for dysphagia, chefs at Aria Care create menus around their likes and dislikes, identifying any modifications that are required for a particular dish. “Presentation is also key,” continues James. “We all eat with our eyes, so we focus on the presentation as well as the taste to ensure residents’ appetites are stimulated by both the look and smells of the foods. With the IDDSI meals, you should always try to replicate the original dish regardless of the IDDSI level to maintain dining quality.”
Regular tasting sessions are another way to keep menus fresh and inviting. “You can gain feedback, interact with those you are cooking for and respond to people,” says Leni. “It is also important to have a tasting session with your kitchen team. The flavour is so important, especially with levels 3,4 and 5.”

